Panic disorder can impair your ability to go to work, enjoy your day, or even stop you from leaving your home. If your panic attacks are so severe that they are disrupting your daily life, it’s important to seek diagnosis and treatment. But how can you know which treatment is right for you? Finding ways to cope with panic disorder can seem overwhelming. Here are ten key points that can help you understand your treatment options for panic disorder.
1. Not All Panic Attacks Lead to a Diagnosis of Panic Disorder
If you are experiencing panic attacks for the first time, it’s important to have a doctor figure out why. Not everyone who has a panic attack develops panic disorder. There are also other health reasons that can cause panic attacks, including medical causes like heart issues, asthma, and hyperthyroidism.
2. You Don’t Have to Choose Between Medication and Therapy
If you have been diagnosed with panic disorder, treatment possibilities can include therapy, medications, or a combination of both. Medication is often most effective when combined with therapy. For treating panic disorder, therapy provides long-term coping skills and tools to manage and reduce panic attacks.
There are several different evidence-based therapies that can be used to treat panic disorder, including Cognitive Behavioral Therapy (CBT), exposure therapy, and mindfulness. These types of therapies—commonly known as “talk therapy”—can be very effective, and people often try talk therapy to see if they can manage their panic disorder without medications. However, for some people, starting with medication can help them achieve enough stability to participate in therapy. Often, after a person has developed the skills to cope with their anxiety, he/she may feel comfortable with stopping medications completely.
3. Find the Right Therapist for You
Choosing the right therapist can be confusing and difficult. First, find a therapist with experience treating anxiety. Therapists come from various fields, including psychiatry, psychology, and clinical social work, and specialize in different types of disorders. Second, find a therapist who provides the services you are looking for.
For example, if you are interested in your medication options, check if the clinician does psychopharmacology evaluations. If you are most interested in structured talk therapy with homework assignments, find a therapist who specializes in Cognitive Behavioral Therapy.
4. Treatment is Based on More Than Just Your Disorder
Ask your provider to consider your personal factors to arrive at a few treatment plan options. Why? Treatment plans should be tailored to each individual because everyone’s situation, needs, and preferences are different. Medication decisions can depend on several personal factors: your immediate and long-term needs, the severity and frequency of your symptoms, your preferences, and your philosophy on medication in general.
It’s helpful to have a therapist or psychiatrist you trust who can integrate your individual needs and preferences into your treatment plan. The hope is that your provider can offer you multiple effective options so that together you can figure out which plan best fits your needs and goals.
5. Know Who can Prescribe Medication for Panic Disorder
In the majority of states, psychiatrists and psychiatric nurses are the only types of therapists who can prescribe medications. In New Mexico and Louisiana, trained psychologists may also be able to prescribe. If you have limited access to mental health specialists in your local area, your primary care physician or family physician may be able to manage and prescribe medications for your anxiety or refer you to a psychiatrist.
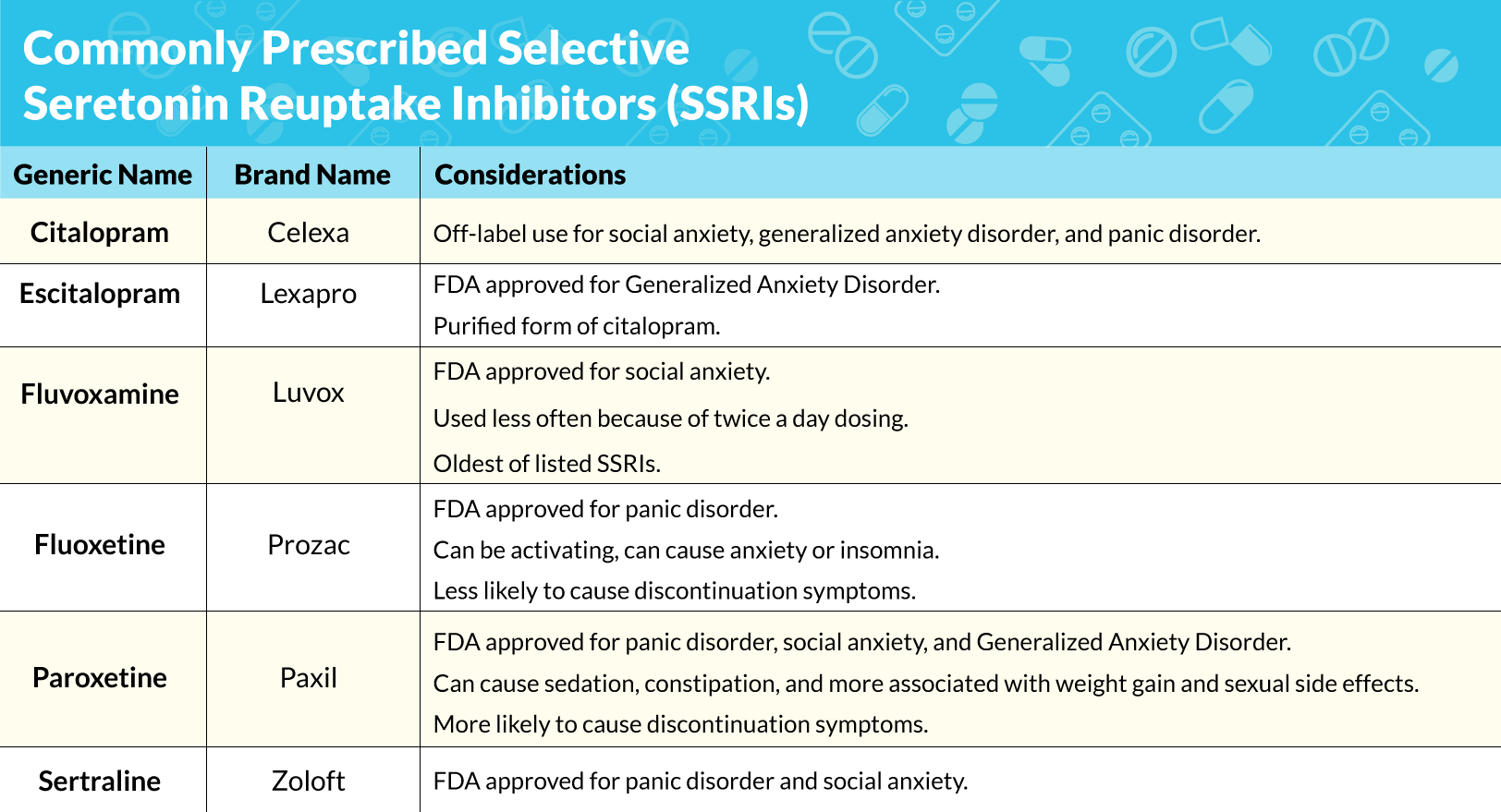
6. Understand SSRIs
The typical initial pharmacologic treatment for panic disorder is a category of medications called selective serotonin reuptake inhibitors (SSRIs). SSRIs can reduce the number and severity of panic attacks as soon as one to two weeks after taking them. SSRIs block the reabsorption of serotonin, leading to changes in the balance of serotonin in the brain. SSRIs are typically prescribed to be taken daily.
They are also used to treat depression. The good thing about SSRIs is that they are non-addictive. However, they aren’t without withdrawal symptoms—you may experience discontinuation symptoms after stopping daily doses, such as mild headache and fatigue for a few days. With this in mind, if you are using an SSRI, it’s best to ask your doctor how to taper the medication safely and gradually.
Commonly Prescribed Selective Serotonin Reuptake Inhibitors (SSRIs)
Common Side Effects of SSRIs:
-
-
- Some of the most common side effects for SSRIs are nausea, headache, jitteriness, and gastrointestinal issues such as cramping or diarrhea. Some of these initial side effects typically go away after a few days and should improve as your body adjusts to the medication. However, if the side effects persist, be sure to discuss them with your doctor.
- Even at low doses, sexual side effects, including lower libido, premature ejaculation, and decreased ability to orgasm in both men and women are common. Discuss this with your doctor.
- Weight gain can occur on SSRIs and varies by individual.
- Uncommon side effects to know about: If you have an immediate reaction after starting the medication, such as difficulty breathing or swelling of your face, oral mucosa, or throat, this requires immediate medical attention. Call 911 or go to the nearest emergency room. If you have any thoughts of harm to yourself or others, then it is important you get emergency care.
-
7. Finding the Right Medication for You Takes Time
If you and your doctor decide to try an SSRI, remember that figuring out which SSRI works best for you can be a long process (think two months or longer). This is because many people need to try different dosages and allow adequate time to pass in order to really tell if the medication is working properly. Some important factors that determine whether the medication is right for you include:
-
- effectiveness
- side effects
- potential drug interactions with other medications you are taking
- cost
All SSRIs are generally equivalent in terms of effectiveness. However, it’s difficult to predict which SSRI will be effective for you or what type of side effects you may experience because every individual reacts differently. Also, certain medications that you are already taking might limit your choice of SSRI. The most commonly prescribed SSRIs (listed in table above) are all available in generic forms and may be covered by your insurance.
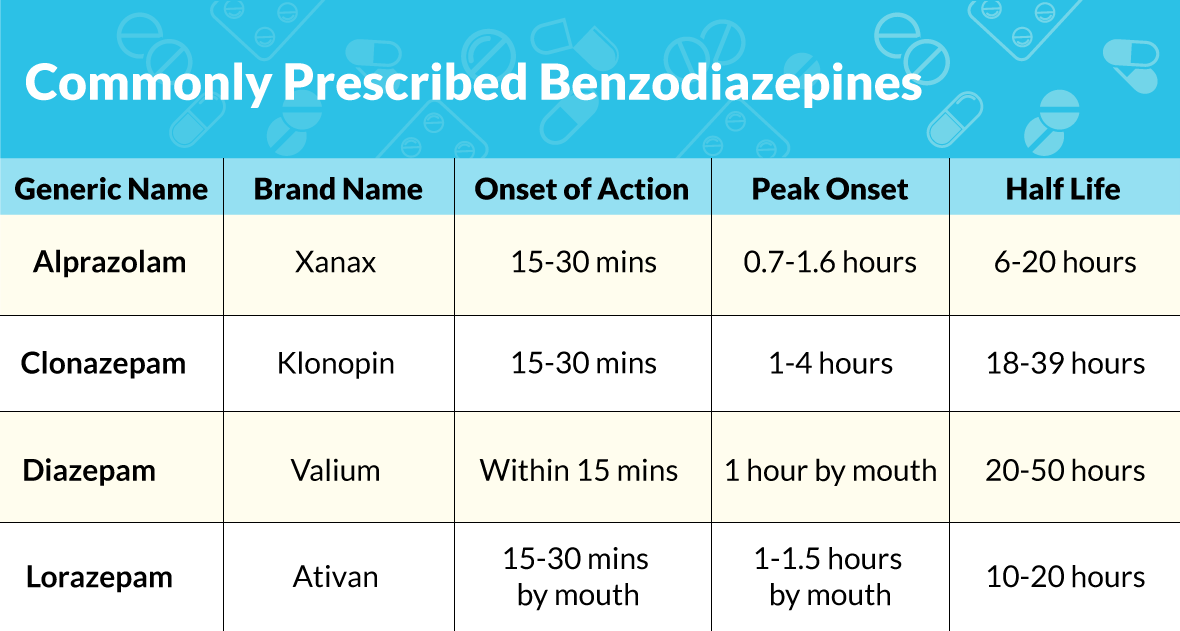
8. Understand Benzodiazepines
Other common medications for anxiety include a category of medications called benzodiazepines. Benzodiazepines may be useful for immediate, short-term relief in panic disorder, but do not provide a long-term strategy by themselves and may not be a good fit for your treatment for other reasons. There are two main issues with benzodiazepines that make them less of an effective long-term medication choice for panic disorder:
-
- Benzodiazepines are very addictive: After regular use of benzodiazepines, your body becomes dependent and will develop tolerance, which means that higher doses will be needed to achieve the same effect.
-
- Benzodiazepines can potentially undermine the practice and development of non-medication coping skills: You do not want to encourage a system of thought or behavior in which the only solution to prevent or get rid of a panic attack is to take a fast-acting medication like a benzodiazepine.
An important part of treatment is overcoming the fear of panic attacks, especially before and as they occur. One difficult aspect of panic episodes is the irrational fear that it will never end, which triggers further catastrophic thinking and escalates the panic attack.
Instead of relying on fast-acting benzodiazepines to achieve instant relief, practicing non-medication coping skills, such as deep-breathing or tracking and analyzing your thought patterns, can be a useful investment in your long-term treatment. Being able to practice these coping skills successfully can help reassure you during future panic attacks.
One intermediary step that is useful (and different from actually taking the benzodiazepine each time you anticipate an attack) is carrying around the medication as a fail-safe. Sometimes, the knowledge that you have a back-up medication can be reassuring enough to prevent panic attacks.
Commonly Prescribed Benzodiazepines
 Common Side Effects of Benzodiazepines:
Common Side Effects of Benzodiazepines:
Common side effects include sleepiness, drowsiness, and dizziness. One should not operate machinery or drive while using benzodiazepines. Alcohol should not be combined with benzodiazepines given the risk of death from overdose, respiratory depression, and sedation.
9. Create Short-Term and Long-Term Goals For Your Treatment
Set both short-term and long-term goals for treatment before you start taking medication. For example, if you are having daily panic attacks, a short-term goal can be to complete a record of each episode, including the triggers as well as your thoughts, emotions, and behaviors. A long-term goal might be to reduce your daily panic attacks to less than once a week in three months. Having both types of goals in your treatment plan can help you keep track of your progress.
Benzodiazepines are generally used for immediate and short-term management and can usually be stopped once symptoms have improved with therapy and SSRIs. In terms of SSRIs, you may want to wait until you have felt 100 percent for six months or longer before considering stopping medication(s).
However, this period may be shorter if stressful circumstances have resolved or if you’ve gained a lot of tools and skills to address the panic attacks without medication(s). If you are thinking about stopping your medication(s), it is important to discuss this with your doctor to avoid any withdrawal or discontinuation symptoms.
10. Keep Track of Your Doses
While SSRIs aren’t habit-forming, benzodiazepines are known to be highly addictive. Because of this, it’s important to be honest with your doctor if you find that you have been using them more often or at higher doses than prescribed. Hopefully, your doctor creates a safe, non-judgmental environment for you to feel like you can be candid about your concerns.
If not, find a doctor you can trust to discuss this issue. Additionally, suddenly stopping benzodiazepines can be dangerous and potentially fatal. Your doctor can design a plan to decrease your dose safely, connect you with support and resources, and discuss alternative, non-addictive medications that can be effective in treating your panic disorder.
From finding a good therapist to understanding the available treatment options, trying to sort through all the parts of getting help for your panic disorder can be tricky. Keeping these tips in mind can help you navigate your path to getting better, encouraging you to stay informed and engaged in the process.
Marlynn Wei, M.D., J.D. is a board-certified psychiatrist and therapist with a private practice based in Manhattan, New York. She is a graduate of the Harvard Medical School Massachusetts General Hospital/McLean Hospital psychiatry program. She received her M.D. from Yale School of Medicine and J.D. from Yale Law School.
Dr. Wei provides a holistic approach, integrating insight-oriented therapy, exercise, yoga, mindfulness, and cognitive behavioral skills. She specializes in treating anxiety and helping clients with self-esteem, relationship, and career issues. She works with high-achieving professionals from a range of fields, including finance, startups, law, and medicine, and works together with clients to reduce stress and improve wellness. She has a special interest in working with those in the creative industry like fine arts, design, acting, filmmaking, music, and writes about the challenges of productivity, expression, and fulfillment.
Dr. Wei has appeared as a featured expert on the Z Living Network’s Yoga Sutra Now and been consulted by Cosmopolitan and New York Daily News on a range of topics, including mindfulness, self-compassion, and yoga for anxiety and sleep. She has several publications, including in the Journal of Health Law and the Massachusetts General Hospital Handbook of General Hospital Psychiatry.



 Common Side Effects of Benzodiazepines:
Common Side Effects of Benzodiazepines: