Symptoms of anxiety can occur at any age, but are often under-recognized and under-treated in people over the age of 65. Primary care and other health specialists may be more attuned to symptoms of depression and miss signs of anxiety, which include physical symptoms such as shortness of breath and difficulty sleeping, as well as cognitive and emotional symptoms such as excessive worrying and irritability.
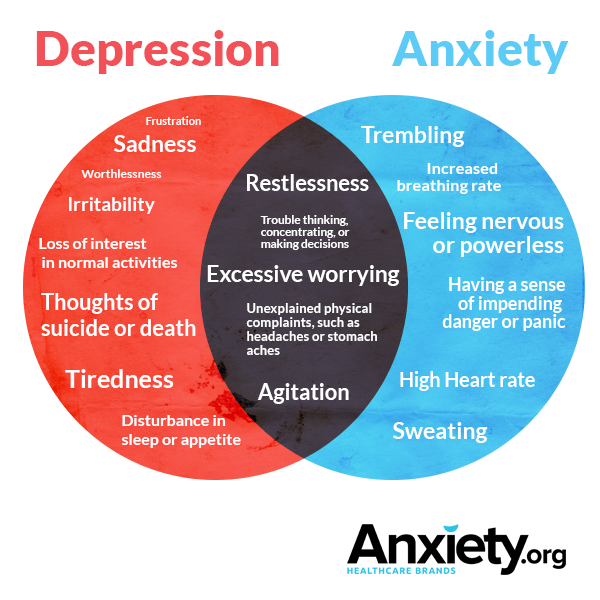
Depression and anxiety have many symptoms in common, including unexplained physical symptoms such as headaches and problems with thinking and memory. Although there are many other shared symptoms, excessive worry, focus on worry, and heightened feelings of anxiety and nervousness are among the primary features which distinguish anxiety from depression. Despite the tendency to under-diagnose, late life anxiety symptoms are actually much more prevalent than depressive symptoms. Though many symptoms are distinctive, common symptoms between the disorders can cause diagnostic errors. See the chart below:
The Effects of Under-Diagnosing Anxiety
Though these two afflictions often overlap, treatment for depression and anxiety can be very different. There are many negative consequences of leaving anxiety undiagnosed and therefore untreated. Untreated individuals are more likely to experience diminished well-being, reduced quality of life, impaired ability to carry out basic activities of daily living, poorer health, and reduced life satisfaction.1,2
Why are Older Adults More Likely to be Misdiagnosed?
Often, older adults experiencing symptoms of anxiety have difficulty communicating their experience. Anxiety symptoms can mimic side effects of medications as well as the symptoms of other disorders. Take, for example, shortness of breath or heart palpitations: each can be a sign of respiratory or cardiac diseases, potential anxiety disorder, or a reflection of the presence of both. With such varying possibilities, it is no wonder both patients and health professionals can mistake symptoms of anxiety for other things, or miss them altogether. Also, changes in memory and increased physical symptoms (such as trembling or headaches) are common in later life, making distinguishing between depression and anxiety even more difficult.
Anxiety Symptoms Present Differently Later in Life
Compared to those afflicted by anxiety at younger ages, older adults with anxiety are more likely to be women and suffering from another illness. Older adults with anxiety also complain of cognitive (e.g., memory and attention) and behavioural (e.g., poorer sleep and appetite) symptoms more often than younger persons suffering from anxiety.
Studies suggest that phobias are the most common anxiety disorder among older people, with Generalized Anxiety Disorder (GAD) being slightly less prevalent in the older population.3 Other anxiety disorders, such as Obsessive-Compulsive Disorder (OCD) and Post-Traumatic Stress Disorder (PTSD), are relatively uncommon in later life.
The Geriatric Anxiety Inventory: Diagnosing Late-Life Anxiety
Proper, specialized anxiety testing can reduce both misdiagnosis and under diagnosis among later-life sufferers. The Geriatric Anxiety Inventory (GAI) is used in many clinical and research settings globally in order to accurately measure late-life anxiety.4 The GAI was developed specifically for use with older adults – the assessment was designed, tested and validated on persons over age 65. The GAI is appropriate for use in a wide range of settings in which health professionals may encounter older patients, including inpatient, community outpatient, and nursing home settings. The instrument was kept relatively brief (20 items) with a simple agree/disagree response format for ease of use with persons with mild cognitive impairment. The GAI is not a diagnostic tool, but rather a means for health professionals to gauge the patient’s symptom severity across a range of anxiety disorders and symptoms. Being able to measure symptoms allows health professionals to know which patients to follow up with for a more comprehensive assessment of anxiety symptoms. It also enables the health provider to reassess symptoms following treatment in order to determine if the intervention is in fact reducing symptoms.
The GAI has been shown to measure psychological distress with excellent reliability and concurrent validity.4 A shortened version of the GAI, with only five items, was developed for use in epidemiological research and as a brief screening tool.5 The assessment has also been translated to over two dozen languages, spread across five continents, with psychometric properties remaining largely consistent across translations.6 This consistency is important as it allows for crucial cross-cultural comparisons of anxiety symptoms in healthy and clinical populations.
The GAI is a useful screening tool that a broad range of health professionals can easily incorporate into their everyday practice in order to provide better detection, treatment, and follow up for debilitating anxiety disorders in later life.
Sources
1Bryant, C., Jackson, H., & Ames, D. 2009. Depression and anxiety in medically unwell older adults: Prevalence and short-term course. International Psychogeriatrics, 21, 754-763.
2Porensky, E. K., Dew, M. A., Karp, J. F., Skidmore, E., Rollman, B. L., Shear, M. K. & Lenze, E. J. 2009. The burden of late-life generalized anxiety disorder: Effects on disability, health-related quality of life, and healthcare utilization. American Journal of Geriatric Psychiatry, 17, 473-482.
3Ritchie, K., Artero, S., Beluche, I., Ancelin, M. L., Mann, A., Dupuy, A. M., … Boulenger, J. P. (2004). Prevalence of DSM-IV psychiatric disorder in the French elderly population: The Esprit Study. British Journal of Psychiatry, 184, 147–152.
4Pachana, N. A., Byrne, G. J., Siddle, H., Koloski, N., Harley. E., & Arnold, E. (2007). Development and validation of the Geriatric Anxiety Inventory. International Psychogeriatrics, 19, 103–114.
5Byrne, G. J. A., & Pachana, N. A. (2011). Development and validation of a short form of the Geriatric Anxiety Inventory: the GAI-SF. International Psychogeriatrics. 23(1), 125-131.
6Pachana, N. A., & Byrne, G. J. (2012). The Geriatric Anxiety Inventory: International use and future directions. Australian Psychologist, 47, 33-38.
Nancy A. Pachana, Ph.D., FAPS, FASSA, is a clinical geropsychologist, neuropsychologist and professor in the School of Psychology at The University of Queensland, and is co-director of the UQ Ageing Mind Initiative. She has an international reputation in the area of geriatric mental health, particularly with her research on late-life anxiety disorders.
She has published over 200 peer-reviewed articles, book chapters and books on various topics in the field of ageing. She received the Inaugural Alastair Heron Prize for Research in Dementia (2006) from the Clinical College of the Australian Psychological Society, and serves on the editorial board of the Journals of Gerontology: Psychological Science, one of the top two journals in the world for publication of research in the science of the psychology of aging.
Dr. Pachana was elected a Fellow of the Academy of Social Sciences in Australia in 2014. Her main research interests include anxiety in later life, psychological interventions for those with Parkinson’s Disease, nursing home interventions and driving safety and dementia. She has recently published the text Assessment and Psychotherapy with Older Adults with her colleague Professor Bob Knight from the University of Southern California.